Parents and carers
This page is for those who have care for a child or young person who has been diagnosed with a lazy eye and/or a squint. It deals with the important role you will play in helping the child or young person to benefit from the treatment they get.
Lazy Eye is more formally known of as Amblyopia. This word means blunt vision. What is really happening is that one eye has a significantly lower power (acuity) than the other.
Why does Amblyopia happen?
New-born babies have poor vision. They must learn to look at an object of interest and to see what they are looking at. This process fails to happen correctly for around one in twenty children and is called a “lazy eye” (amblyopia). When one eye is long-sighted or short-sighted relative to the other (called anisometropia) the child will develop impaired vision in that eye, or less commonly in both. The same problem arises when one eye looks in a different direction to the other - this is called a squint or strabismus. Anisometropia and strabismus frequently occur together, but can also develop on their own to produce amblyopia. Our aim is to provide new ways of improving the treatment of amblyopia and strabismus, compared to conventional methods.
What do we do?
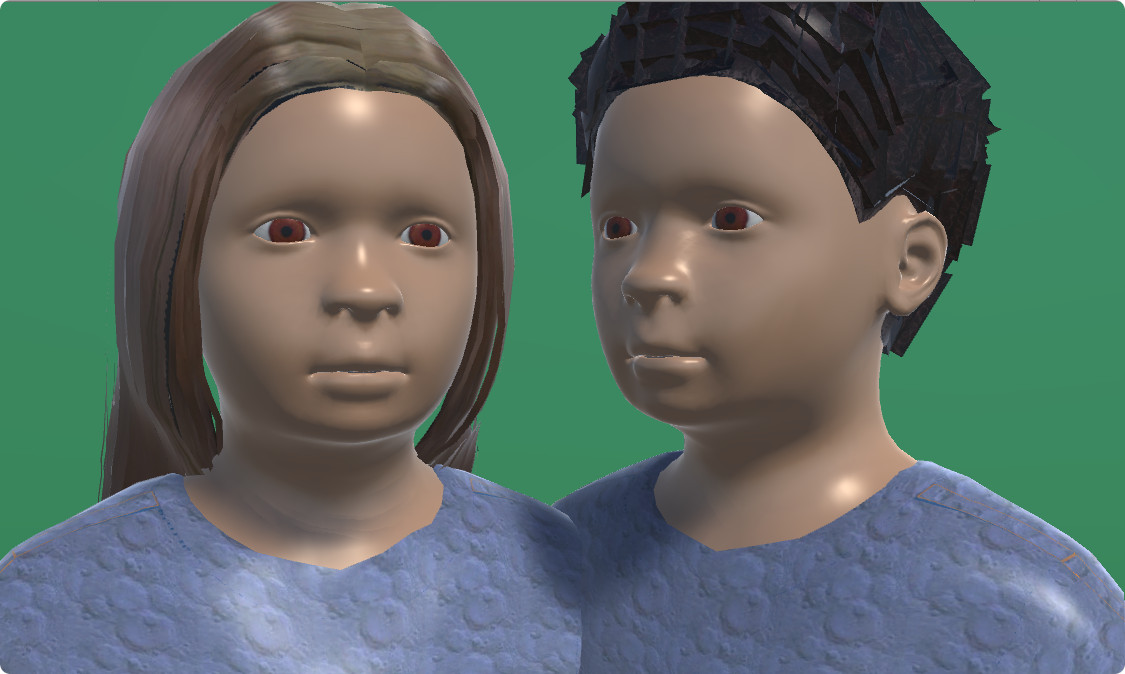
We have developed methods of treatment that are more convenient for the patient and will provide more reliable results than with more traditional approaches. Our software, and the hardware it comes on, do not replace the clinician role - rather they enhance it. The traditional treatment for amblyopia is a two-stage process in some cases. First, the child wears glasses for a period of up to 3 months. If the amblyopia is not resolved, as is the case for around 2/3 of patients, or the child does not require glasses, then patching of the better eye is initiated. Instead of patching some patients may be treated by use of eye drops to “blur” the vision of the better seeing eye. One problem with patching and blurring is that patients find it uncomfortable and as a result treatment compliance can be poor. Patching also has the additional problem that the patch is obvious to the child's peers and can often lead to bullying, anxiety and low self esteem. The treatment we provide for amblyopia involves playing specially adapted computer games and watching age appropriate videos. In the games, different parts of the same image are presented to either eye. The big advantage over patching (and blurring) is that it allows the brain to learn to use visual information from both eyes together. There are various issues which can be individually addressed by using certain combinations of components which are shown to each eye.
In principle, the use of fun and engaging games increases the willingness of the children to comply with the treatment. However, children's computer games are sophisticated, and their game preferences can change frequently. Further, there are certain games which are very popular with children but are not easy to make available within our system (e.g. Minecraft). To fix this, we have focused on adding ways in which children can engage with material they supply - both videos and online games. Both games and videos can be adapted by displaying them uninterrupted to the amblyopic eye while blurring the central focus for the better eye. In this way, a much wider variety of captivating material can be used and the children's compliance with the treatment increased.
Regarding the treatment of Strabismus (squints), especially when present with Amblyopia, a major problem lies with the image from the squinting eye being supressed by the brain. This normally leads to a loss of binocularity. Strabismus is usually treated by corrective surgery. A problem arises when this is done with an eye which is being supressed - after correction, the eye will, in time, go out of alignment again (in 80% of cases). Our system can be combined with the use of corrective surgery and enable treatment to help break suppression. It is well demonstrated that when post operation the patient has a good level of binocularity that the probability of the squint recurring and the need for further realignment surgery is greatly reduced. In addition our equipment can be used to provide entertaining exercises within games that will help to align the eyes.
Are we the only people using games? If not what is special about us?
The simple answer to the first of these questions is no. While we were responsible for the first demonstrated practical use of these techniques, others have been following our lead. However, we have completed clinical trials with funding originally from the Wellcome Trust and later from the UK National Institute for Health Research (NIHR), which have given us greater insight into what works and what does not. In particular, we have been working closely with ophthalmic surgeons to demonstrate how we can reduce the need for subsequent realignment surgery in patients with strabismus.
Our system uses an eye-tracker to monitor eye position and allows us to preferentially stimulate the lazy eye. We are currently trialling this system for children with a lazy eye. Because lazy eye and squint often occur together it makes sense to treat both at the same time. The eye-tracker allows us to establish how well both eyes are working together and the device provides exercises to enhance this. Unlike traditional treatment approaches, which restricts input to one eye in favour of the other, we actively promote using both eyes together. This allows the good eye to act as a template for recovering functional vision in the lazy eye.